
DANGERS OF ACTINIC KERATOSIS (AK)
A potential unseen threat of skin cancer1-3,†
What is actinic keratosis (AK)?
Actinic keratoses are premalignant lesions of the skin that, when left untreated, can potentially develop into squamous cell carcinoma (SCC), the second most common form of skin cancer. AK is primarily caused by chronic sun damage and generally affects people aged 40 or older.1,4
Could you be at risk?
- More than a third of the general population over the age 51 has at least 1 AK lesion that may be found on their head or scalp.5 If left untreated, AKs of any severity can develop into a skin cancer called SCC. SCC is the second most common form of skin cancer.1,6
What are the signs of AK?
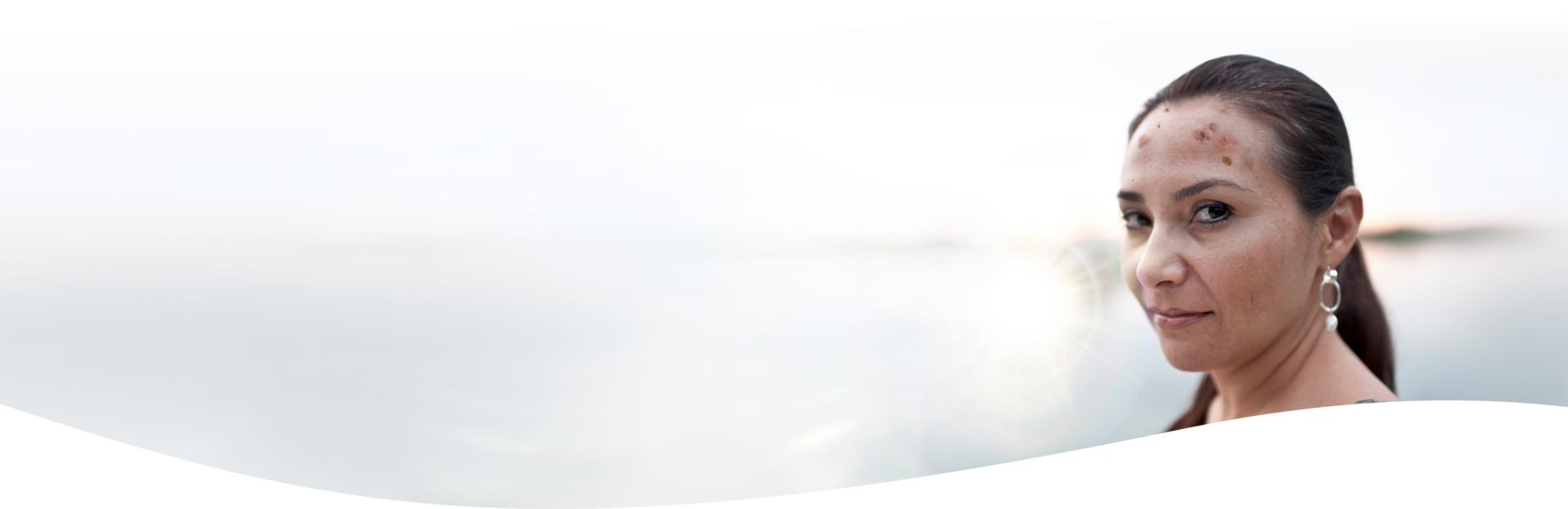
AK lesions typically form on areas of the body most exposed to the sun—such as the face and scalp. AK lesions can have a different clinical appearance. They are frequently scaly, range from normal skin color to reddish brown, and can be identified by sight and/or touch.1,2
Because AKs originate in the skin layers below the visible surface, lesions can be present but still difficult to spot. For every visible lesion within a sun-damaged area, there are likely other AKs that are easier felt than seen. Together, these lesions are considered a field.2,3,7
If you have concerns that you may have AK, please talk with your healthcare provider.
For every AK lesion you can see, there are likely more lesions that you can feel but may be difficult to see.3,8


AKs are among the most common conditions for which patients visit their dermatologists.9
Learn how your healthcare provider can treat mild-to-moderate AK on your face and scalp.
Questions
If you have any questions about AMELUZ®, please contact your healthcare provider.

DANGERS OF ACTINIC KERATOSIS (AK)
A potential unseen threat of skin cancer1-3,†
What is actinic keratosis (AK)?
Actinic keratoses are premalignant lesions of the skin that, when left untreated, can potentially develop into squamous cell carcinoma (SCC), the second most common form of skin cancer. AK is primarily caused by chronic sun damage and generally affects people aged 40 or older.1,4
Could you be at risk?
- More than a third of the general population over the age 51 has at least 1 AK lesion that may be found on their head or scalp.5 If left untreated, AKs of any severity can develop into a skin cancer called SCC. SCC is the second most common form of skin cancer.1,6


What are the signs of AK?
AK lesions typically form on areas of the body most exposed to the sun—such as the face and scalp. AK lesions can have a different clinical appearance. They are frequently scaly, range from normal skin color to reddish brown, and can be identified by sight and/or touch.1,2
Because AKs originate in the skin layers below the visible surface, lesions can be present but still difficult to spot. For every visible lesion within a sun-damaged area, there are likely other AKs that are easier felt than seen. Together, these lesions are considered a field.2,3,7
If you have concerns that you may have AK, please talk with your healthcare provider.
For every AK lesion you can see, there are likely more lesions that you can feel but may be difficult to see.3,8



AKs are among the most common conditions for which patients visit their dermatologists.9
Learn how your healthcare provider can treat mild-to-moderate AK on your face and scalp.
Questions
If you have any questions about AMELUZ®, please contact your healthcare provider.

DANGERS OF ACTINIC KERATOSIS (AK)
A potential unseen threat of skin cancer1-3,†
What is actinic keratosis (AK)?
Actinic keratoses are premalignant lesions of the skin that, when left untreated, can potentially develop into squamous cell carcinoma (SCC), the second most common form of skin cancer. AK is primarily caused by chronic sun damage and generally affects people aged 40 or older.1,4
Could you be at risk?
- More than a third of the general population over the age 51 has at least 1 AK lesion that may be found on their head or scalp.5 If left untreated, AKs of any severity can develop into a skin cancer called SCC. SCC is the second most common form of skin cancer.1,6


What are the signs of AK?
AK lesions typically form on areas of the body most exposed to the sun—such as the face and scalp. AK lesions can have a different clinical appearance. They are frequently scaly, range from normal skin color to reddish brown, and can be identified by sight and/or touch.1,2
Because AKs originate in the skin layers below the visible surface, lesions can be present but still difficult to spot. For every visible lesion within a sun-damaged area, there are likely other AKs that are easier felt than seen. Together, these lesions are considered a field.2,3,7
If you have concerns that you may have AK, please talk with your healthcare provider.
For every AK lesion you can see, there are likely more lesions that you can feel but may be difficult to see.3,8



AKs are among the most common conditions for which patients visit their dermatologists.9
Learn how your healthcare provider can treat mild-to-moderate AK on your face and scalp.
Questions
If you have any questions about AMELUZ®, please contact your healthcare provider.
INDICATION AND IMPORTANT SAFETY INFORMATION
INDICATION
AMELUZ® (aminolevulinic acid hydrochloride) topical gel, 10%, a porphyrin precursor, in combination with photodynamic therapy using BF-RhodoLED® or RhodoLED® XL lamp, is indicated for the lesion-directed and field-directed treatment of actinic keratoses of mild-to-moderate severity on the face and scalp.
IMPORTANT SAFETY INFORMATION
AMELUZ® (aminolevulinic acid hydrochloride), topical gel, 10%
Purpose: Photosensitizing agent
Uses: AMELUZ® gel, a porphyrin precursor, in combination with photodynamic therapy using BF-RhodoLED® or RhodoLED® XL lamp, is used for lesion-directed and field-directed treatment of actinic keratoses of mild-to-moderate severity on the face and scalp.
Warnings:
Do not use if you have a:
- Known hypersensitivity to photoactive substances known as porphyrins.
- Known hypersensitivity to soybeans.
- Known hypersensitivity to any component of AMELUZ®.
Ask your Health Care Provider before use If you have:
- Porphyria (hereditary disease that is characterized by abnormal production of a red blood pigment called heme).
- Photodermatoses (skin conditions caused by or made worse by exposure to light or ultraviolet radiation).
When using this product:
- Allergic reactions: AMELUZ® may cause allergic reactions before photodynamic therapy. AMELUZ® should be washed off and suitable treatment started. The allergic reactions can potentially include severe courses like sudden, severe allergic reaction with breathing difficulty, swelling, lightheadedness, fast heartbeat, sweating and loss of consciousness.
- Transient Amnestic Episodes: Photodynamic therapy may cause transient amnestic episodes (temporary loss of memory). If observed, the therapy must be stopped immediately. If observed after treatment, contact your health care provider.
- Risk of Eye Injury: Patients and health care providers must wear protective eyewear while operating BF-RhodoLED® or RhodoLED® XL.
- Photosensitivity: Avoid sun exposure on the treated lesion sites and surrounding skin for approximately 48 hours following treatment.
- Risk of Bleeding: Special care should be taken to avoid bleeding during lesion preparation in patients with inherited or acquired coagulation disorders. Bleeding must be stopped before application of the gel.
- Ophthalmic Adverse Reactions: Avoid applying AMELUZ® into the eyes. Wash eyes with water in case of accidental contact.
- Mucous Membrane Irritation: Avoid direct contact of AMELUZ® with the mucous membranes. Wash with water in case of accidental contact.
- Concomitant use of the following medications may increase the intensity of adverse reactions after light exposure related to photodynamic therapy: St. John’s wort, griseofulvin, thiazide diuretics, sulfonylureas, phenothiazines, sulphonamides, quinolones, and tetracyclines.
Most common side effects at the application site were:
- skin reddening
- pain/burning
- irritation
- swelling
- itching
- scaling of the skin
- scabbing
- hardening
- blistering
Most side effects occurred during illumination or shortly afterwards, were generally of mild or moderate intensity, and lasted for 1 to 4 days in most cases; in some cases they persisted for 1 to 2 weeks or even longer.
Pregnancy Warning: There is no available data on AMELUZ® use in pregnant women to inform a drug associated risk.
Lactation Warning: There is no available data regarding the presence of the active ingredient (aminolevulinic acid hydrochloride) in human milk, or the effects of aminolevulinic acid hydrochloride on the breastfed infant or on milk production.
Pediatric Warning: Safety and effectiveness in pediatric patients below the age of 18 has not been established.
Geriatric Warning: No overall differences in safety or effectiveness were observed between older (65 years and older) and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Directions:
- AMELUZ® is administered only by a health care provider.
- AMELUZ® is for topical use only.
- Photodynamic therapy with AMELUZ® involves preparation of lesions, application of the product, occlusion and illumination with BF-RhodoLED® or RhodoLED® XL.
- Retreat lesions that have not completely resolved 3 months after the initial treatment.
Inactive Ingredients: xanthan gum, soybean phosphatidylcholine, polysorbate 80, medium-chain triglycerides, isopropyl alcohol, dibasic sodium phosphate, monobasic sodium phosphate, sodium benzoate and purified water.
Other Information:
- Store in a refrigerator, 2°C – 8°C (36°F – 46°F). Excursions permitted to 15°C – 30°C (59°F – 86°F).
- The risk information provided here is not comprehensive. To learn more, talk about AMELUZ® with your health care provider. The FDA approved product labeling can be found at https://www.ameluz.com/PI.
- You are encouraged to report side effects of AMELUZ®. Please contact Biofrontera Inc. at 1-844-829-7434 or FDA at 1-800-332-1088 or www.fda.gov/medwatch.
References: 1. Reinhold U. A review of BF-200 ALA for the photodynamic treatment of mild-to-moderate actinic keratosis. Future Oncol. 2017;13(27):2413-2428. 2. Stockfleth E. The importance of treating the field in actinic keratosis. J Eur Acad Dermatol Venereol. 2017;31(Suppl 2):8-11. 3. Berman B, Amini S, Valins W, Block S. Pharmacotherapy of actinic keratosis. Expert Opin Pharmacother. 2009;10(18):3015-3031. 4. Actinic keratosis risk factors. Skin Cancer Foundation. Updated January 2022. Accessed August 12, 2024. https://www.skincancer.org/skin-cancer-information/actinic-keratosis/causes-and-risk-factors/. 5. Flohil C, van der Leest R, Dowlatshahi E, Hofman A, de Vries E, Nijsten T. Prevalence of actinic keratosis and its risk factors in the general population: the Rotterdam Study. J Invest Dermatol. 2013;133(8):1971-1978. 6. Fernández-Figueras MT, Carrato C, Sáenz X, et al. Actinic keratosis with atypical basal cells (AKI) is the most common lesion associated with invasive squamous cell carcinoma of the skin. J Eur Acad Dermatol Venereol. 2015;29:991-997. 7. Cockerell CJ. Histopathology of incipient intraepidermal squamous cell carcinoma ("actinic keratosis"). J Am Acad Dermatol. 2000;42(1 Pt 2):11-7. 8. Olsen EA, Abernethy L, Kulp-Shorten C, et al. A double-blind, vehicle-controlled study evaluating masoprocol cream in the treatment of actinic keratoses on the head and neck. J Am Acad Dermatol. 1991;24:738-43. 9. Grada A, Muddasani S, Fleischer AB, et al. Trends in office visits for the five most common skin diseases in the United States. J Clin Aesthet Dermatol. 2022;15(5):E82-E86.
